It’s Food Allergy Awareness Week May 9-15th, so we share each day of that week content and news you can use. What better way to honor this week and all those living with food allergies than by presenting a (remarkably brief) overview of our amazing immune system and how food allergies work. Our immune system is a complicated interconnected array of many moving parts. A comprehensive review of every aspect is well beyond the scope of this blog, and many textbooks for that matter. We’ll touch on the important parts specific to food allergies.

To start, there are two major divisions of our immune systems which are tightly connected: the innate and the adaptive immune systems. Think of the innate immune system as your first line of defense. It is the barrier to the external world that protects you from invaders. This is your skin, the lining of your airways and gut, as well as many specialized cells that react in the event of an infection or injury. Your adaptive immune system, as the name suggests, is the part that learns and maintains an “infection memory” so that future similar infections can be handled quickly and effectively. When your innate immune system fails, the adaptive kicks in to mount the attack on foreign particles.
Foreign particles are called antigens in the immunology world. An antigen is anything that can be identified by the immune system as non-self. In the case of food allergies, these are specific proteins that are unique to a given food. Antigens can be obtained and presented by the innate to the adaptive immune system and trigger an immune response to clear the body of potential threats. The response is tightly regulated so that we may carry on day to day. If the body had an allergic reaction to every single antigen encountered, we would not survive.

Let’s say you have a peanut allergy, for example. You accidentally eat a salad dressing that has peanut ingredients. What happens? Special cells in the lining of the gut called mast cells detect the presence of the peanut antigen. They attach to this antigen and present it to the immune system. They can also release certain chemicals into the body to mediate an immune response. You’ve probably heard of histamine. When the peanut antigen binds to these mast cells, they release histamine which has a cascading effect on the body, and results in what we consider to be an allergic reaction.
So why do only some antigens, like certain peanut proteins, trigger these responses? There is a special molecule called an antibody (not to be confused with antigen), that binds to mast cells. There are several different types of antibodies, the one we are concerned with in terms of food allergies is called IgE. There are many varieties of IgE which only bind to certain antigens. One may bind to peanut antigens, while another may bind to soy antigens, another binds to shellfish antigens, and so forth. IgE is present on mast cells as well as free floating in the bloodstream. And when you have an antigen-IgE-mast cell combination, chemicals such as histamine are released. When histamine is released, there is an allergic reaction.
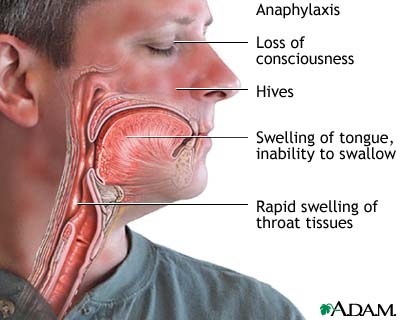
What happens when there is an allergic reaction? Typically, it is not an emergency, maybe a runny nose or skin rash. It is when there is an exaggerated release of histamine that a potentially life-threatening condition called anaphylaxis can occur. Anaphylaxis is characterized by low blood pressure and a weak rapid pulse, constricted airways, diarrhea and vomiting, hives or itching, and potentially shock. Because it can affect the ability to breathe, anaphylaxis needs to be treated right away. The first treatment is epinephrine, which is another name for adrenaline (that’s right, the fight-or-flight hormone).
Epinephrine opens the airways to help with breathing and constricts the blood vessels which helps skin symptoms like swelling and redness. It addresses the symptoms of a severe allergic reaction; it does not reverse the causes. So, it is important to seek medical attention following administering epinephrine for follow up treatment and observation.
There is currently no known treatment for food allergies other than eliminating the troublesome foods from the diet. If someone has a severe food allergy and are at risk for anaphylaxis, they should carry an epinephrine pen with them in the event of accidental exposure. The human immune system is an amazing defense that protects us all day every day. But with so many intricate parts and interactions, it is easy to see how an error upstream can have serious effects.



